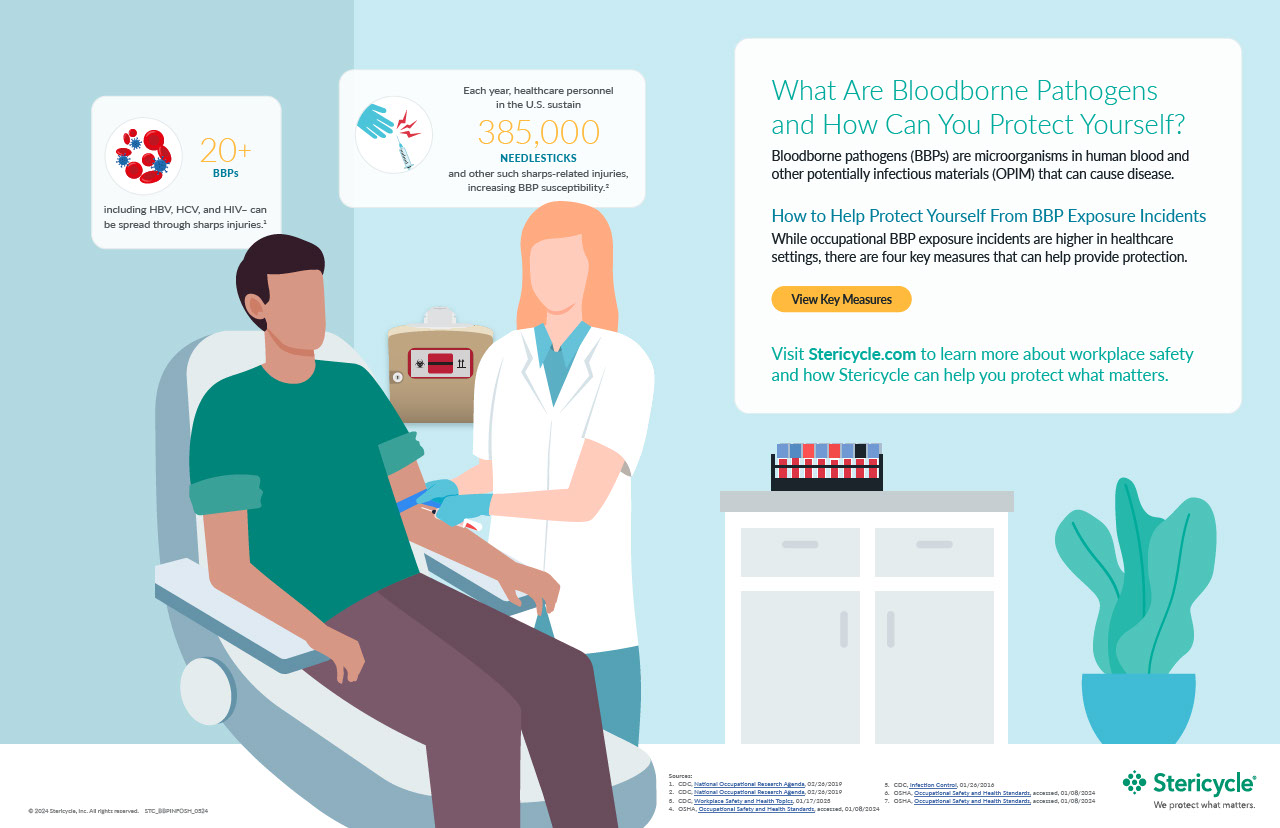
Occupational exposure to bloodborne pathogens (BBPs) poses a significant risk to healthcare personnel, with an estimated 385,000 needlesticks and other sharps-related injuries occurring annually. These exposure incidents are associated with occupational transmission of hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV), as well as more than 20 other pathogens.
There are safety controls and workplace practices that can be implemented to eliminate or reduce the chances of BBP exposure incidents. It is important to learn how to protect your employees and prevent potential exposure incidents in any healthcare setting, whether you are a large hospital or small medical practice.
What are Bloodborne Pathogens (BBPs)?
Bloodborne pathogens are pathogenic microorganisms found in human blood and other potentially infectious materials (OPIM) that have the potential to cause diseases in humans. These pathogens include viruses and bacteria that can be transmitted from one person to another through exposure to infected blood or OPIM. The most common bloodborne pathogens include:
- Hepatitis B Virus (HBV): A viral infection that attacks the liver and can be an acute short-term illness or become a long-term chronic infection. HBV is transmitted from a person who has an infection to a person who is not infected through activities that involve percutaneous or mucosal contact with infectious blood or body fluids. Chronic HBV can lead to life-threatening health issues like liver disease or liver cancer.
- Hepatitis C Virus (HCV): A viral infection that attacks the liver and can be an acute short-term illness or become a long-term chronic infection. HCV is usually spread when someone comes into contact with blood from an infected person, commonly from a contaminated needle. More than half of people who become infected with HCV will develop a chronic infection, which can lead to life-threatening health issues like liver disease or liver cancer.
- Human Immunodeficiency Virus (HIV): A virus that attacks the body’s immune system, causing chronic long-term infections. If HIV is not treated, it can lead to advanced stage disease known as AIDS (acquired immunodeficiency syndrome). HIV can be transmitted through blood or infectious bodily fluids when they come in contact with a mucous membrane or damaged tissue or are directly injected into the bloodstream (from a needle or syringe).
A Path to Prevention: Following OSHA’s Bloodborne Pathogen Standard
Prevention of BBP exposure incidents is an attainable goal. It begins with a commitment by healthcare facilities and personnel to adhere to the requirements outlined in the Occupational Safety and Health Administration’s (OSHA) Bloodborne Pathogen Standard.
This standard prescribes a framework for reducing and preventing BBP exposure incidents and outlines requirements necessary to safeguard healthcare workers. Requirements include establishing exposure plans, implementing administrative and engineering controls, providing comprehensive training to employees, and ensuring the availability and use of personal protective equipment (PPE):
- Engineering Controls: An engineering control isolates or removes a hazard. Engineering controls can come in the form of safer devices such as compliant sharps containers or safety needles to reduce or eliminate the chance of an exposure incident.
- Work Practice Controls: Changing the way a task is performed to reduce the likelihood of exposure to blood or OPIM. Facilities should put workplace safety rules in place, such as prohibiting the recapping of needles by a two-handed technique. OSHA’s BBP Standard requires following OSHA’s Universal Precautions, which is defined as treating human blood and specific body fluids (OPIM) as already being infectious; however, it is highly recommended to follow CDC’s Standard Precautions, which treat all bodily fluids as potentially infectious.
- Administrative Controls: Includes policies, procedures and plans to keep employees safe from injury and illness:
- Develop a BBP Exposure Control Plan detailing how an organization prevents exposure to bloodborne pathogens and what’s involved in responding to a BBP exposure incident should one occur. The document should describe training programs, HBV vaccination protocol, engineering controls that reduce risk, and more.
- Provide training to any employee who has anticipated exposure to human blood or OPIM. BBP training must occur at the time of initial job assignment and at least annually thereafter. Stericycle’s online training module can help your staff understand the BBP standard and can help meet the standard’s training requirements.
- Establish recordkeeping protocols to track and properly document employee BBP exposure incidents.
- Follow OHSA’s requirements for ensuring compliant biohazard warning labels are affixed to containers of regulated waste, refrigerators and freezers containing blood or OPIM, and other containers used to store, transport, or ship blood and OPIM.
- Personal Protective Equipment (PPE): Using PPE to protect workers from BBP hazards is imperative. OSHA’s BBP standard 29 CFR 1910.1030 contains PPE requirements for occupational exposure to blood and OPIM including, but not limited to, hand, face, eye, and body protection.
By implementing the requirements prescribed by OSHA in the BBP standard, healthcare professionals can significantly reduce the number of preventable needlesticks and sharps-related injuries on the job and subsequent BBP exposure incidents.
How Stericycle Can Help Organizations Reduce BBP Exposure Incidents
As an industry leader, Stericycle is a committed partner in healthcare workplace safety, offering comprehensive OSHA compliance and training programs in the BBP area, including:
- Comprehensive OSHA Compliance: Leverage tailored programs to help ensure your organization meets OSHA's BBP requirements.
- Specialized Training: Equip your staff with the knowledge and skills needed to navigate BBP risks confidently.
- Proactive Risk Minimization: Collaborate with Stericycle to develop a proactive approach to minimize risks and enhance workplace safety.
A proactive approach to healthcare safety should be non-negotiable. A comprehensive strategy that combines adherence to guidelines, robust engineering and administration controls, and the diligent use of personal protective equipment can mitigate the risks posed by BBP exposure incidents.
Stericycle can be a valuable resource in helping your organization minimize risks and develop the necessary elements to achieve and sustain compliance with OSHA’s BBP requirements. Learn how our OSHA Compliance and Training programs can help keep your staff safe and your organization in compliance today and in the future.