Most healthcare workers (88% of providers and 84% of administrators) surveyed in Stericycle’s 2022 Healthcare Workplace Safety Trend Report agree that at-home health care is a growing trend that offers patients select and diversifying services in the comfort of their own homes. Providers understand that at-home care can provide patients comfort (78%), convenience (71%), and personalized care (60%).
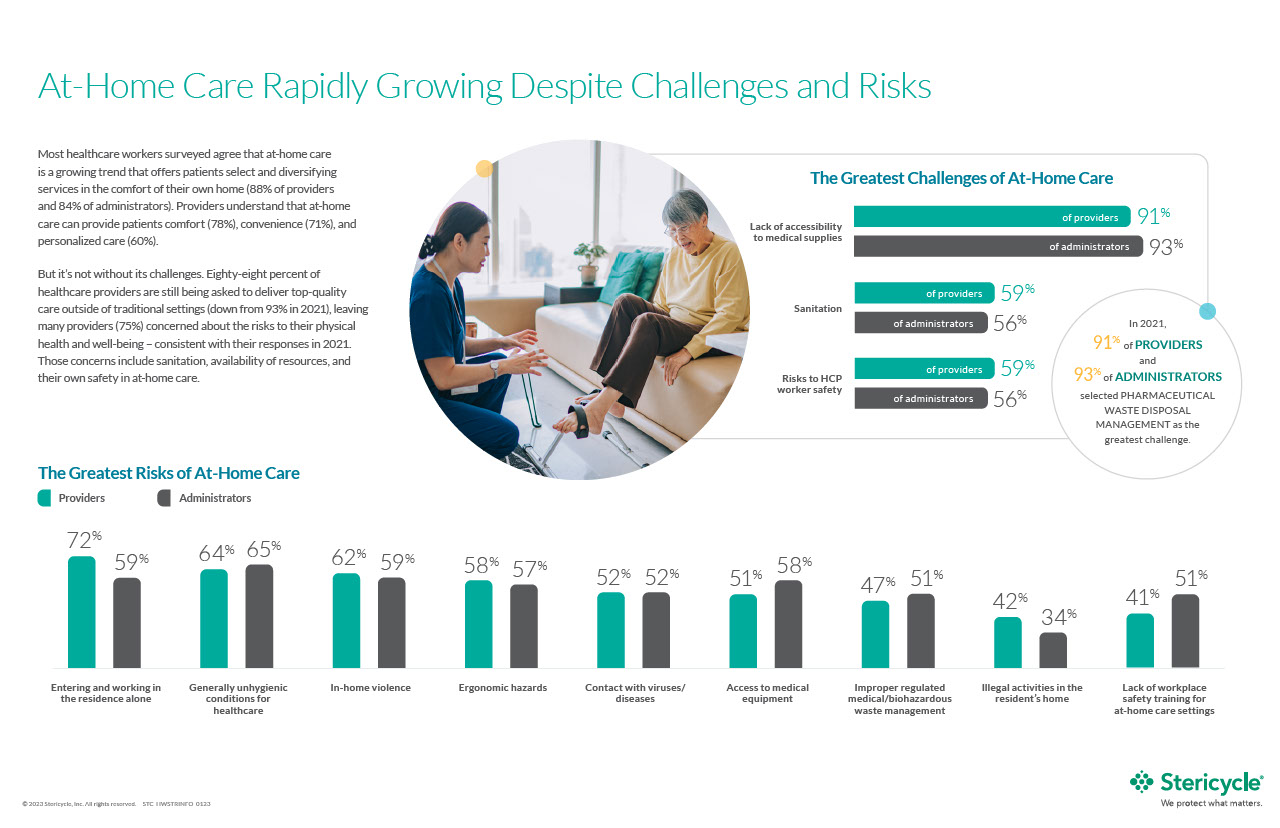
There are challenges, however, to this crucial healthcare service. Eighty-eight percent of healthcare providers surveyed, report that they are still being asked to deliver top-quality care outside of traditional settings, leaving many providers (75%) concerned about the risks to their physical health and well-being — this statistic is consistent with responses in 2021. Those concerns include sanitation, availability of resources, and their own safety as at-home care providers.
Whereas hospitals and other designated healthcare facilities have defined protocols and procedures, at-home health care may not always be as clear. This is a growing concern, given that the population potentially needing this type of support is increasing, and baby boomers make up the second largest age group in the United States population, followed by millennials. This age group requires more healthcare options closer to, or inside, their homes.
Unlike traditional healthcare facilities, at-home care providers have little control over their work environments and can be exposed to unsafe working conditions such as unsanitary homes, temperature extremes, homes without safe drinking water, or hostile pets. The Occupational Safety and Health Administration (OSHA) outlines other hazards that can exist in home healthcare settings that can negatively impact patients, providers, and the communities they live in. Some of these hazards include:
Bloodborne pathogens: These infectious microorganisms found in human blood can cause disease in humans. Pathogens include, but are not limited to, hepatitis B (HBV), hepatitis C (HCV), and human immunodeficiency virus (HIV). Bloodborne pathogens such as HBV, HCV, and HIV can be transmitted through contact with infected human blood and other potentially infectious materials. Bloodborne pathogens are most commonly transmitted in healthcare settings through:
- Accidental puncture from contaminated needles, broken glass, or other sharps
- Contact between broken or damaged skin and infected body fluids
- Contact between mucous membranes and infected body fluids
Occupational exposure to bloodborne pathogens from needlesticks and other sharps injuries is a serious problem across hospital-based healthcare personnel; there are approximately 385,000 needlesticks and other sharps-related injuries each year. Healthcare workers must be aware of the potential risks of disease from these commonly used supplies. At-home caregivers share the same risks as hospital or clinic-based providers but may not have the same resources for injuries if they occur.
Biological hazards: Regulated medical waste (RMW), which includes biohazardous, biomedical, infectious, or regulated medical waste as defined under federal, state, or local law, is another key hazard for at-home healthcare.
RMW is a waste or reusable material derived from the medical treatment of an animal or human that is known to contain or potentially contain a pathogen. For this reason, providers and administrators should be familiar with proper RMW disposal methods.
Latex sensitivity: Frequent exposure to the natural rubber of latex, often found in medical gloves, can lead to potential allergies. There are several types of reactions that can occur:
- Irritant contact dermatitis is the most common reaction, indicated by dry, itchy, and irritated skin.
- Allergic contact dermatitis, otherwise known as delayed hypersensitivity, is a more delayed reaction, often showing up 24 to 96 hours after contact with the allergen.
- Latex allergy, otherwise known as immediate hypersensitivity, may entail serious symptoms that require medical attention. This reaction could occur within minutes, but symptoms may also take up to a few hours to develop. More mild symptoms are redness and itching, while more serious symptoms can manifest themselves in the form of sneezing, coughing, a scratchy throat, and more. Any serious reactions should be treated by a medical professional.
Ergonomic hazards: The physical health and efficiency of healthcare services may be impacted from lifting or transporting a patient. Chances of injury are increased if there is no assistive equipment or other forms of guidance to help with mobility.
In 2018, nationally, there were 49,040 reported injuries and illnesses among home health care aides. There are many resources available to assist in assessing and reducing home healthcare workers' risks for workplace injury and illness. The Centers for Disease Control and Prevention’s National Institute for Occupational Safety and Health (NIOSH), in partnership with OSHA, offers a free and active curriculum for at-home healthcare safety. The Training for Homecare Workers, titled Caring for Yourself While Caring for Others, aims to encourage practices that bolster the health and safety of providers and patients. Further, The Homecare Workers’ Handbook is an easy-to-read overview of some of the topics covered in this course.
Learn more about the challenges and risks of at-home care by downloading Stericycle’s infographic.