Opioids are often an effective and important part of patient care, but there can be unintended consequences such as the opioid epidemic. More than one million people began pain reliever misuse in 2020, and over 16,000 Americans die from prescription-opioid-related deaths annually.
Hospital costs for patients who experience opioid overdoses are estimated upwards of 11 billion dollars annually. Layer in the COVID-19 pandemic on top of public health and cost implications, and it’s easy to understand why the opioid epidemic is a top concern for healthcare leaders.
Healthcare facilities are uniquely positioned to help combat the opioid epidemic, and healthcare leaders have taken steps toward mitigating risks in prescribing opioids. These efforts include prescription drug monitoring programs, implementing clinical guidelines for assessing the prescribing of opioids, and providing medical professionals with continuing education courses focused on pain treatment.
The Role of Drug Diversion in the Opioid Epidemic
While tactics have increased to monitor and curb prescribing controlled substances, there is another contributor to the opioid epidemic—drug diversion. Drug diversion, or the redirecting of controlled substances by staff or patients from their intended destination for illicit distribution or use, is often a threat. It can have broad implications for a healthcare facility and its surrounding community. In addition to negatively impacting well-being and trust, some consequences can include damaged careers, civil and criminal penalties, infectious disease outbreaks, severe patient harm, and even death.
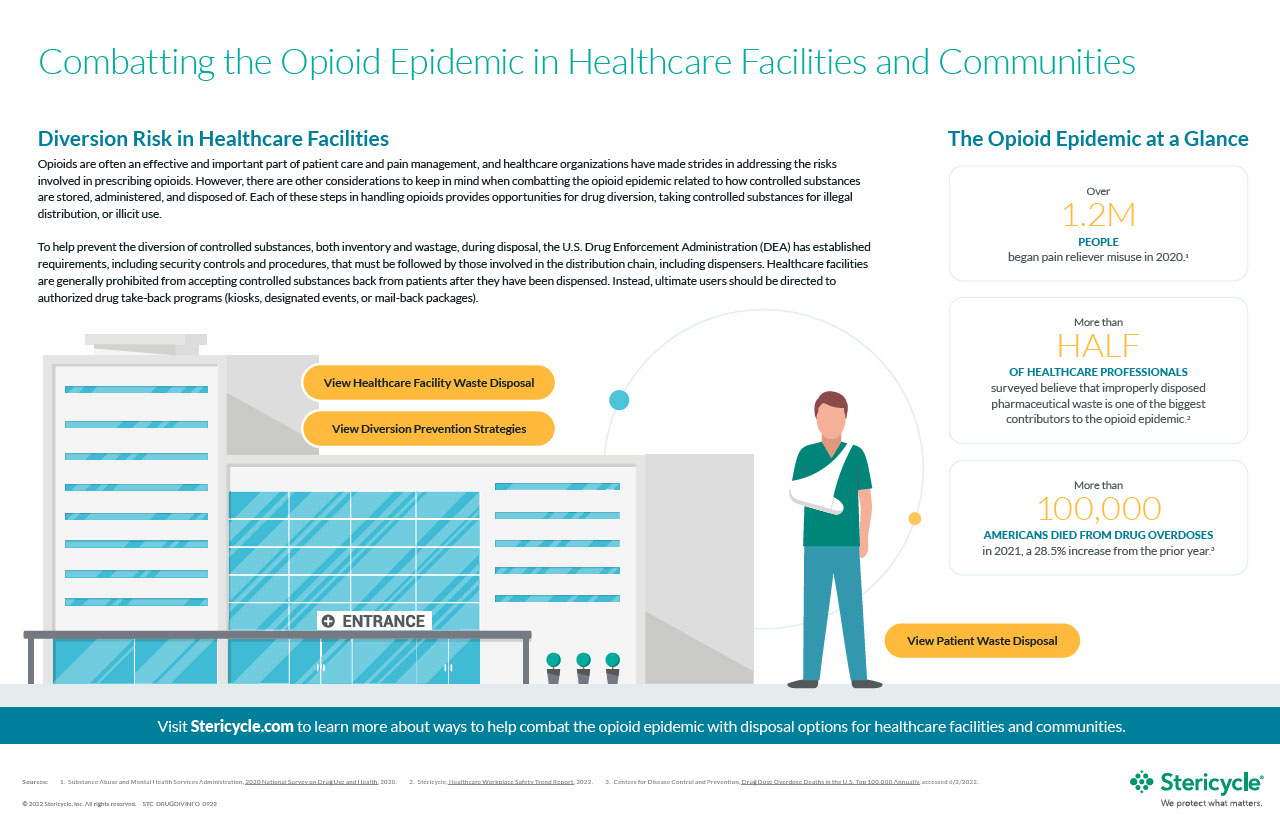
All healthcare organizations are a target for drug diversion. Healthcare facilities should pay careful attention to the processes and procedures they have to store, administer, and dispose of controlled substances. According to Stericycle’s Healthcare Workplace Safety Trend Report, over half of the healthcare workers (56%) surveyed believe improperly disposed pharmaceutical waste is one of the top contributors to the opioid epidemic. Furthermore, some experts believe that wasting, or the process of disposing excess medication from a vial or a syringe, is most vulnerable to diversion and should have the proper mitigations strategies in place.
Common Misconceptions about Drug Diversion
While considered a high-risk area, many may believe that drug diversion is an activity that only occurs in hospitals. However, non-acute care facilities can also be vulnerable as they may have fewer resources to monitor and detect diversion. Therefore, long-term care facilities, outpatient clinics, and veterinary clinics should also have mitigation strategies.
It is not always easy to spot drug diversion, and many experts believe that detection and reporting are underestimated. Under reporting may be due to a reluctance from staff to consider their co-workers in that light and bring their suspicions forward. But early identification is crucial, and healthcare staff can play a critical role in detection. Some flags that diversion is potentially occurring include tampered packaging, excessive use, and false documentation.
Misuse of controlled substances can also happen outside the four walls of a healthcare facility. A JAMA Internal Medicine Research Letter highlights that most non-medical users of prescription opioids surveyed receive them from a friend or relative. In a survey from the Centers for Medicare and Medicaid Services (CMS), 60-70% of teens surveyed indicated that medicine cabinets are the source of their drugs. Regardless, easy access to prescription pain relievers should be addressed to help stop drug diversion.
What Can Healthcare Facilities Do to Combat Diversion?
Through implementation of a combination of both internal and patient-facing policies, healthcare organizations can do their part to help stop illegal drug diversion practices. A drug diversion prevention strategy should include:
- Policy Implementation: With the creation of clear and readily available policy, employees will be better able to avoid both intentional and unintentional drug diversion practices.
- Training: Team members must understand how to properly mitigate drug diversion through best practices, prevention understanding, and correct pharmaceutical waste disposal methods.
- Physical Controls: Make disposal containers available to staff to capture wastage and mitigate diversion.
- Periodic Auditing: Regularly monitor and ensure staff follow procedures and training.
- Patient Training: Implement authorized drug take-back programs for leftover medications.
How to Dispose of Controlled Substances
Controlled substances are drugs regulated by the Drug Enforcement Administration (DEA) and are organized by the risk of their potential for abuse or harm. Many prescription opioids are classified as either Schedule II or Schedule III, meaning that they have a potential for abuse, which may lead to psychological or physical dependence ranging from moderate to high levels.
When disposing of controlled substances, it is important to understand that they cannot be discarded into the same containers as regulated medical waste (red bag or sharps container). Industry best practice for wastage (what is left over after a controlled substance has been administered to a patient) is to use a specially designed receptacle that deactivates the drug and ensures it cannot be retrieved after disposal.
There are also safe practices for patients who can dispose of controlled substances at home, which allow healthcare organizations to help mitigate the risk of drug diversion that may happen once prescriptions leave their facility. These include making drug mail back envelopes and drug collection kiosks available to patients. Drug take back days are also a way to encourage patients to safely dispose of their unused controlled substances.
Strategies to help prevent and detect drug diversion are critical to protecting patients and employees. By creating effective programs for drug diversion prevention, healthcare facilities can assist in combating the opioid epidemic. Learn more about ways to help combat the opioid epidemic with disposal options for healthcare facilities and communities.